
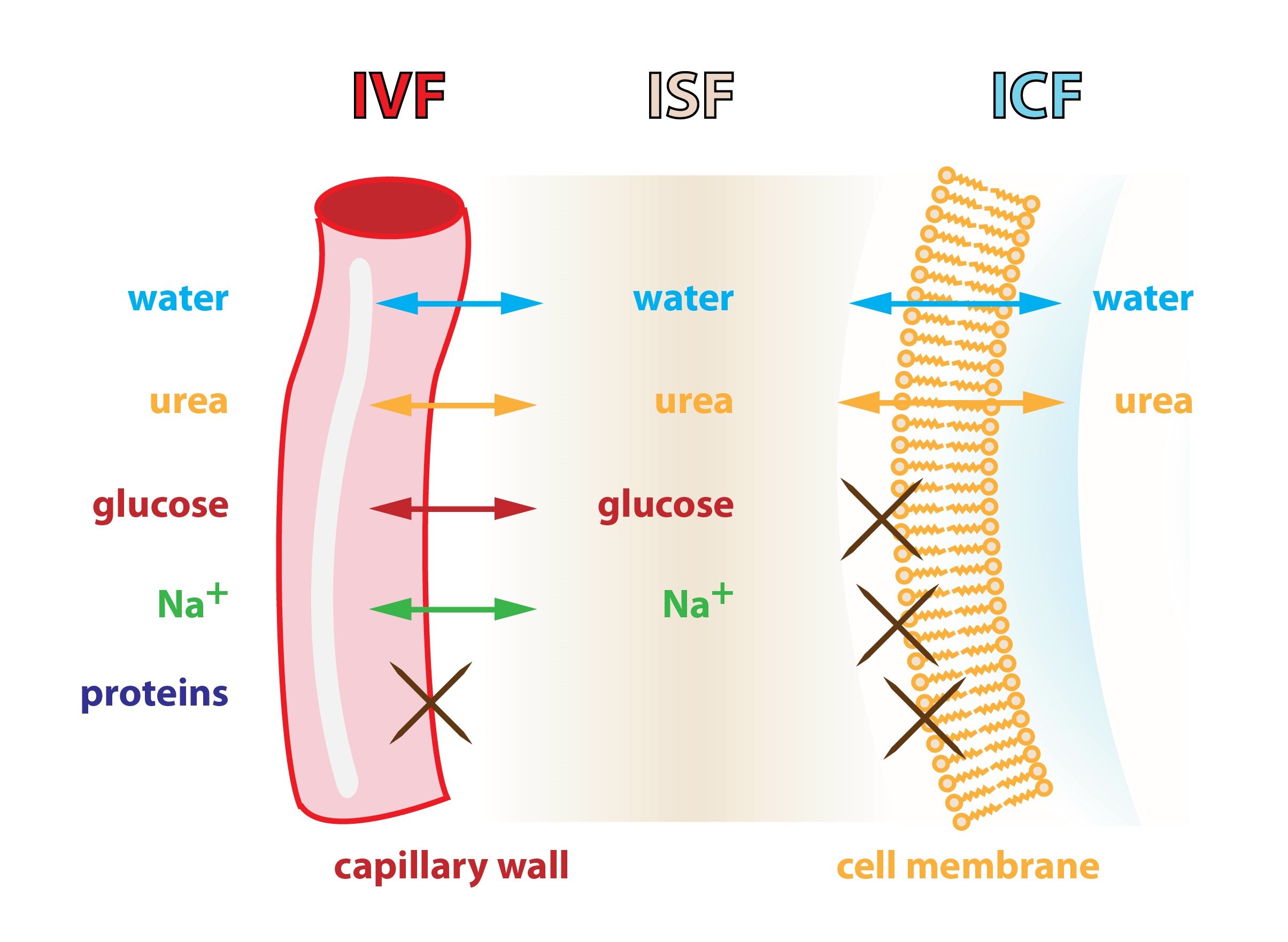
Yet, the regulation of BP is a highly complex, multi-facet interplay between renal, neural, cardiac, vascular, and endocrine factors under the influence of genetic and environmental factors ( 1). Lastly, there is now evidence that sodium can affect the gut microbiome, and induce pro-inflammatory and immune responses, which might contribute to the development of salt-sensitive hypertension.īlood pressure (BP) may appear as a very simple physiological parameter defined as the product of cardiac output and peripheral arterial resistance. In this new model, the immune system plays a role, thereby supporting many previous studies indicating that the immune system is a crucial co-contributor to the maintenance of hypertension through pro-hypertensive effects in the kidney, vasculature, and brain. These observations prompted the refinement of the original model of regulation of sodium balance from a two-compartment model comprising the extracellular fluid within the intravascular and interstitial spaces to a three-compartment model that includes the intracellular space of some tissues, most prominently the skin.
#BODY FLUID COMPARTMENTS YOUTUBE OSMOSIS SKIN#
The first is the discovery made possible with by new technology, such as 23Na-MRI, that sodium can be stored non-osmotically in tissues including the skin and muscles particularly when subjects are on a high sodium diet or have a reduced renal capacity to excrete sodium. In recent years, several new advances were made in our understanding of the interaction between sodium and blood pressure regulation.

Service of Nephrology and Hypertension, Department of Medicine, Centre Hospitalier Universitaire Vaudois, Lausanne, SwitzerlandĪ precise maintenance of sodium and fluid balance is an essential step in the regulation of blood pressure and alterations of this balance may lead to the development of hypertension.Erietta Polychronopoulou, Philippe Braconnier and Michel Burnier *


 0 kommentar(er)
0 kommentar(er)
